Alcohol and esophageal squamous cell carcinoma in east Africa
A large multi-center study across three countries in east Africa confirms the significant role that alcohol intake plays in the public health burden of esophageal squamous cell carcinoma in these countries, particularly among men.
Lancet Glob Health. 2022 Feb;10(2):e236-e245. doi: 10.1016/S2214-109X(21)00506-4. Epub 2021 Dec 15.
Alcohol consumption and oesophageal squamous cell cancer risk in east Africa: findings from the large multicentre ESCCAPE case-control study in Kenya, Tanzania, and Malawi
Daniel R S Middleton 1, Blandina T Mmbaga 2, Diana Menya 3, Charles Dzamalala 4, Gissela Nyakunga-Maro 2, Peter Finch 5, Yohannie Mlombe 4, Joachim Schüz 1, Valerie McCormack 6, ESCCAPE
PMID: 34921758
Abstract
Background: The contribution of alcohol to the large burden of oesophageal squamous cell carcinoma (ESCC) in east Africa remains uncertain and difficult to assess owing to complex consumption patterns of traditional and commercial drinks. We aimed to assess whether alcohol drinking, overall and at specific intake levels, contributes to ESCC risk in east Africa.
Methods: We did a hospital-based case-control study in Kenya, Tanzania, and Malawi, which included comprehensive assessment of a variety of locally consumed alcohol that we used to classify drinkers as exclusively low alcohol-by-volume (ABV; <30% ABV) drinkers or drinkers of some high-ABV drinks, as well as the number of drinks consumed, average weekly ethanol intake, and the contribution of each drink type to overall ethanol consumption. Cases were patients aged 18 years and older with incident primary ESCC, confirmed histologically for the majority of cases, and a clinical diagnosis for the remainder. Controls were frequency-matched on age and sex in a 1:1 ratio with cases. The controls were recruited from the same hospitals as cases and included outpatients, inpatients, and hospital visitors who did not have cancer or any other digestive disease. Consenting participants took part in face-to-face interviews in which they were asked whether they had ever consumed alcohol (the primary exposure variable); those who had were asked follow-up questions about their consumption habits for different alcoholic drinks.
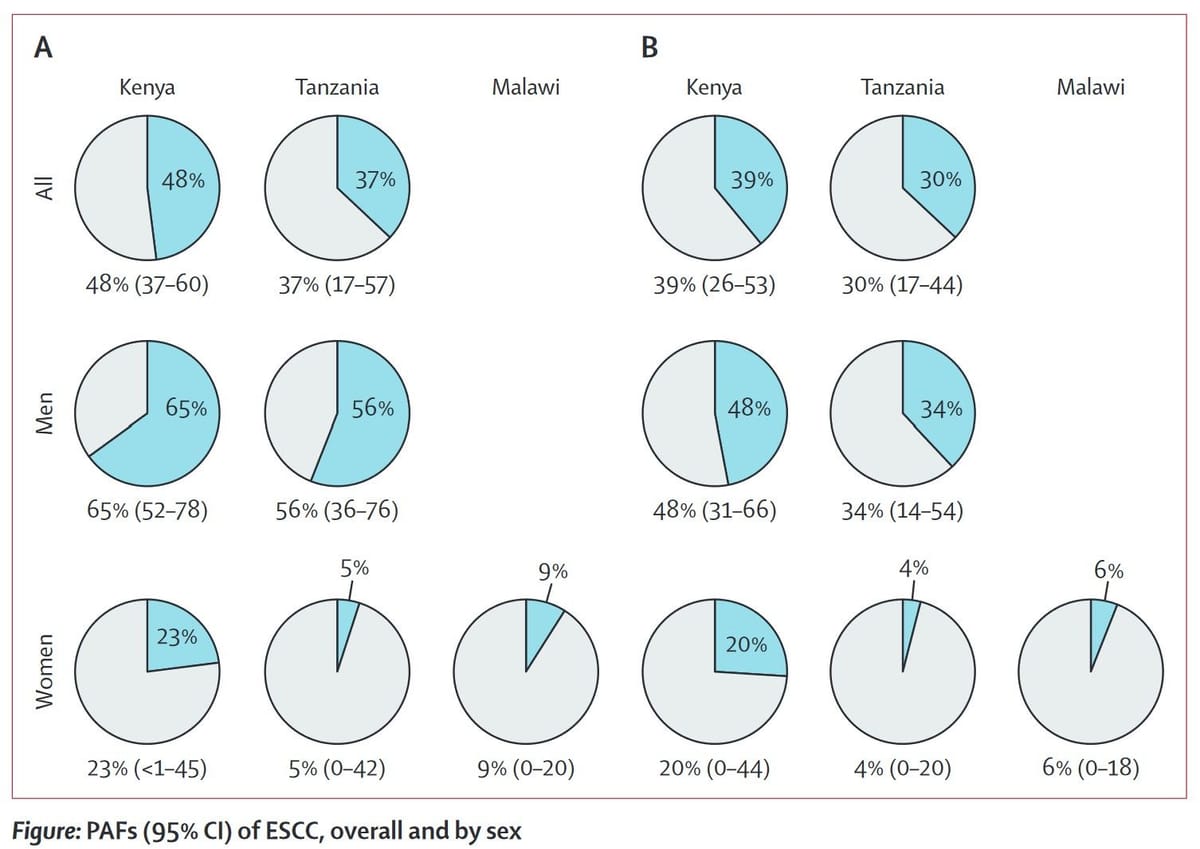
Findings: 1279 cases and 1346 controls were recruited between Aug 5, 2013, and May 24, 2020, including 430 cases and 440 controls from Kenya, 310 cases and 313 controls from Tanzania, and 539 cases and 593 controls from Malawi. 65 (4·8%) of 1344 cases were excluded. Consistent positive associations with ESCC risk were found for ever having consumed alcohol in Kenyan men and Tanzanian men, and for daily number of drinks and estimated ethanol intake in Kenya, Tanzania (both sexes) and Malawian women. Corresponding population-attributable fractions of ESCC for those reporting ever drinking alcohol (vs never drinking) were 65% (95% CI 52-78) in Kenyan men and 23% (<1-45) in Kenyan women, and 56% (95% CI 36-76) in Tanzanian men and 5% (0-42) in Tanzanian women. Increased risk and population-attributable fractions were almost entirely due to risks in high-ABV drinkers.
Interpretation: Alcohol appears to be a substantial contributor to ESCC risk in east Africa, particularly among men, and a large fraction of ESCC could be prevented by cessation or reduction of alcohol consumption. Future studies should consider independent ascertainment of alcohol intake to assess the potential of under-reporting in Malawi.