Bariatric surgery and risk of esophagogastric carcinoma
This study aimed to investigate whether bariatric surgery is associated with an increased risk of developing esophagogastric carcinoma, using a retrospective design and data from a very large national administrative database of hospital discharges in France. The analysis revealed that bariatric surgery was not associated with an additional risk of gastroesophageal carcinoma and was, in fact, associated with a decreased risk of gastroesophageal cancer throughout the spectrum of bariatric procedures. While the study provides reassurance of the protective clinical benefits of weight loss surgery, the authors acknowledge some important limitations, including the lack of histological data on the specific cancers observed, the relatively young age of the participants, and the short overall follow-up duration. When examined by site of origin, cancers located in the lower third of the esophagus (where most adenocarcinomas arise) and the gastric cardia were somewhat more common in the surgical group, suggesting caution in the interpretation of risks for those cancers. It should be noted that the number with unspecified site was quite high, though. The authors suggest that more large-scale studies are needed to focus on the clinical paradox of esophagogastric protection for operations that may increase GERD and to better identify and address the pathophysiological processes of bariatric procedures.
Risk of Esophageal and Gastric Cancer After Bariatric Surgery
Andrea Lazzati 1 2, Tigran Poghosyan 3 4 5, Marwa Touati 6, Denis Collet 7, Caroline Gronnier
Abstract
Importance: Bariatric surgery has been associated with a reduced risk of cancer in individuals with obesity. The association of bariatric surgery with esophageal and gastric cancer is still controversial, however.
Objective: To compare the incidence of esophageal and gastric cancer between patients with obesity who underwent bariatric surgery and those who did not (control group).
Design, setting, and participants: This cohort study obtained data from a national discharge database, including all surgical centers, in France from January 1, 2010, to December 31, 2017. Participants included adults (aged =18 years) with severe obesity who underwent bariatric surgery (surgical group) or who did not (control group). Baseline characteristics were balanced between groups using nearest neighbor propensity score matching with a 1:2 ratio. The study was conducted from March 1, 2020, to June 30, 2021.
Exposures: Bariatric surgery (adjustable gastric banding, gastric bypass, and sleeve gastrectomy) vs no surgery.
Main outcomes and measures: The main outcome was incidence of esophageal and gastric cancer. A secondary outcome was overall in-hospital mortality.
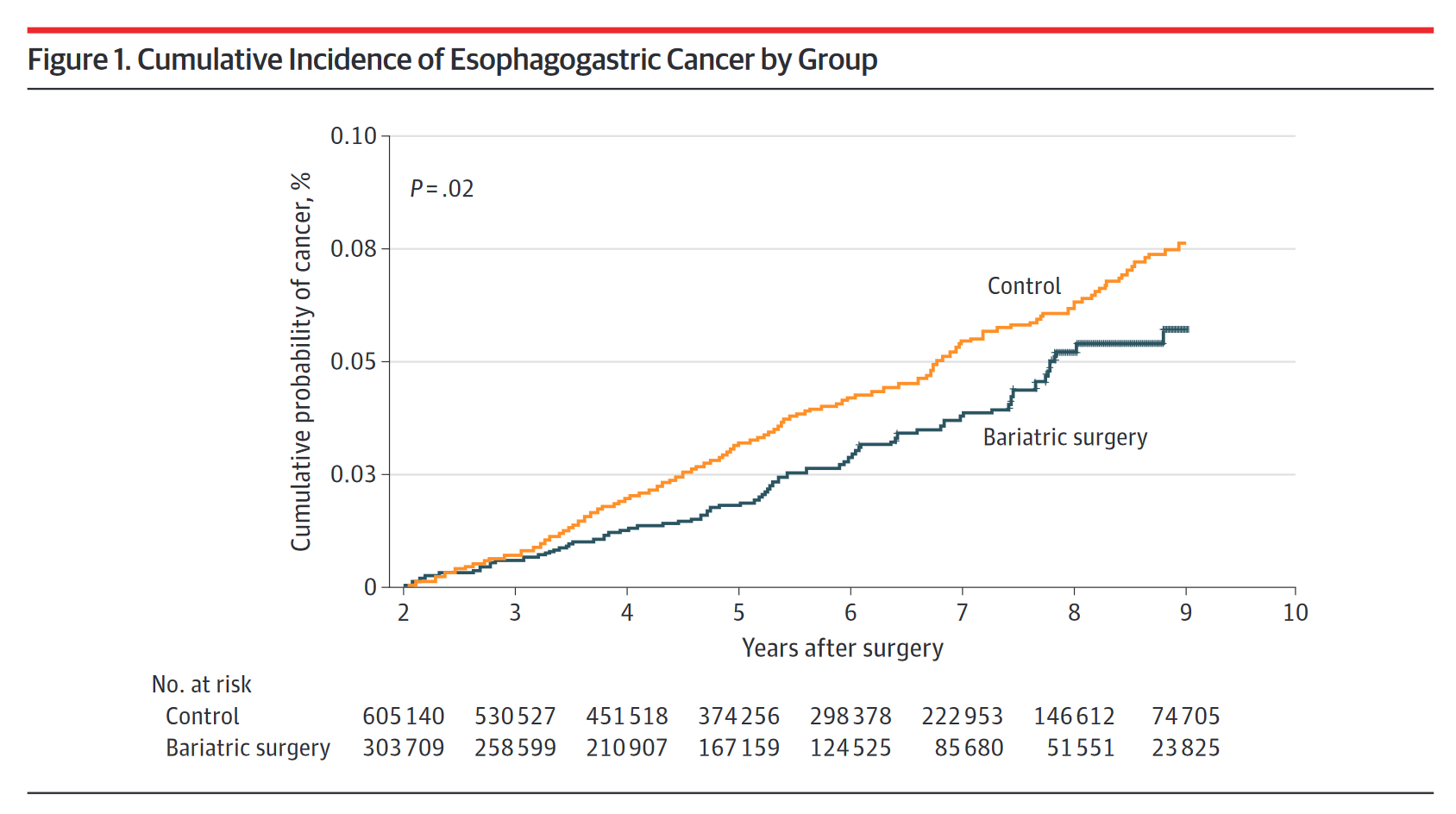
Results: A total of 303 709 patients who underwent bariatric surgery (245 819 females [80.9%]; mean [SD] age, 40.2 [11.9] years) were matched 1:2 with 605 140 patients who did not receive surgery (500 929 females [82.8%]; mean [SD] age, 40.4 [12.5] years). After matching, the 2 groups of patients were comparable in terms of age, sex, and comorbidities (standardized mean difference [SD], 0.05 [0.11]), with some differences in body mass index. The mean follow-up time was 5.62 (2.20) years in the control group and 6.06 (2.31) years in the surgical group. A total of 337 patients had esophagogastric cancer: 83 in the surgical group and 254 in the control group. The incidence rates were 6.9 per 100 000 population per year for the control group and 4.9 per 100 000 population per year for the surgical group, resulting in an incidence rate ratio of 1.42 (95% CI, 1.11-1.82; P = .005). The hazard ratio (HR) of cancer incidence was significantly in favor of the surgical group (HR, 0.76; 95% CI, 0.59-0.98; P = .03). Overall mortality was significantly lower in the surgical group (HR, 0.60; 95% CI, 0.56-0.64; P < .001).
Conclusions and relevance: In this large, nationwide cohort of patients with severe obesity, bariatric surgery was associated with a significant reduction of esophageal and gastric cancer incidence and overall in-hospital mortality, which suggests that bariatric surgery can be performed as treatment for severe obesity without increasing the risk of esophageal and gastric cancer.