Childhood obesity and subsequent esophageal cancer risk
Dr. Petrick and colleagues reported on childhood obesity and subsequent risk of esophageal and gastric cancer in over 60,000 young Danish men. This is one of the first studies that indicate that reduction in obesity between childhood and adulthood may reduce subsequent risk.
Obesity (Silver Spring). 2019 Aug 5. doi: 10.1002/oby.22570. [Epub ahead of print]
Overweight Patterns Between Childhood and Early Adulthood and Esophageal and Gastric Cardia Adenocarcinoma Risk.
Petrick JL, Jensen BW, Sørensen TIA, Cook MB, Baker JL.
Abstract
OBJECTIVE:
Esophageal adenocarcinoma (EA) and gastric cardia adenocarcinoma (GCA) are among the most rapidly increasing cancers in Western countries. Elevated BMI in adulthood is a known risk factor, but associations in early life are unclear.
METHODS:
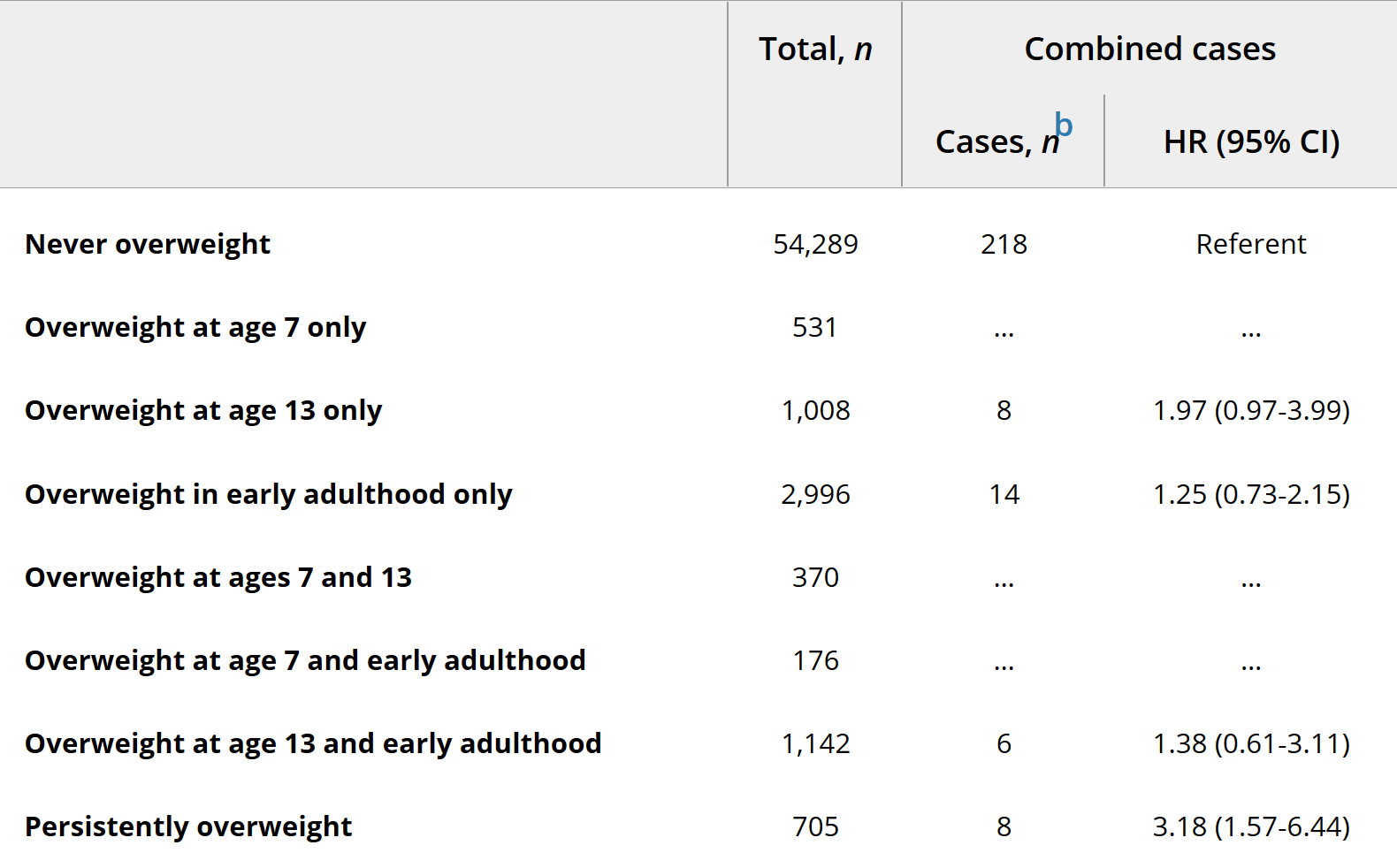
This study assessed weight change between childhood and early adulthood in relation to EA/GCA. Measured weights and heights during childhood (7-13 years) and early adulthood (17-26 years) were available for 64,695 young men from the Copenhagen School Health Records Register and the Danish Conscription Database. Individuals were categorized as having normal weight or overweight. Linkage with the Danish Cancer Registry identified 275 EA/GCA cases. Hazard ratios (HR) and 95% CI were estimated using Cox proportional hazards regression.
RESULTS:
The risk of EA/GCA was 2.5 times higher in men who were first classified as having overweight at age 7 (HR = 2.49; 95% CI: 1.50-4.14) compared with men who were never classified as having overweight. Men who had persistent overweight at ages 7 and 13 and in early adulthood had an EA/GCA risk that was 3.2 times higher (HR = 3.18; 95% CI: 1.57-6.44). However, there was little evidence of increased EA/GCA risk for men with overweight during childhood and subsequent remittance by early adulthood.
CONCLUSIONS:
Persistent overweight in early life is associated with increased EA/GCA risk, which declines if body weight is reduced.