Cost-effectiveness modeling suggests more targeted screening for esophageal adenocarcinoma
Given that the incidence of esophageal adenocarcinoma in the U.S. varies dramatically by sex and race, it seems likely that optimal screening programs might vary as well. CISNET investigators used comparative cost-effectiveness analysis to identify optimal ages for screening by sex and race. Among white men, they found that screening those with GERD at ages 45 and 60 was optimal, whereas black men, who have substantially lower incidence, were best served by a single screening of those with GERD at age 55. In contrast no strategy emerged as optimal in white or black women. Sensitivity analyses revealed alternative stragies for all but black females, whose incidence is currently so low that screeing might cause net harm.
Endoscopic Screening Program for Control of Esophageal Adenocarcinoma in Varied Populations: A Comparative Cost-Effectiveness Analysis
Joel H Rubenstein 1, Amir-Houshang Omidvari 2, Brianna N Lauren 3, William D Hazelton 4, Francesca Lim 3, Sarah Xinhui Tan 3, Chung Yin Kong 5, Minyi Lee 6, Ayman Ali 7, Chin Hur 3, John M Inadomi 8, Georg Luebeck 4, Iris Lansdorp-Vogelaar 2
PMID: 35364064 DOI: 10.1053/j.gastro.2022.03.037
Abstract
Background & aims: Guidelines suggest endoscopic screening for esophageal adenocarcinoma (EAC) among individuals with symptoms of gastroesophageal reflux disease (GERD) and additional risk factors. We aimed to determine at what age to perform screening and whether sex and race should influence the decision.
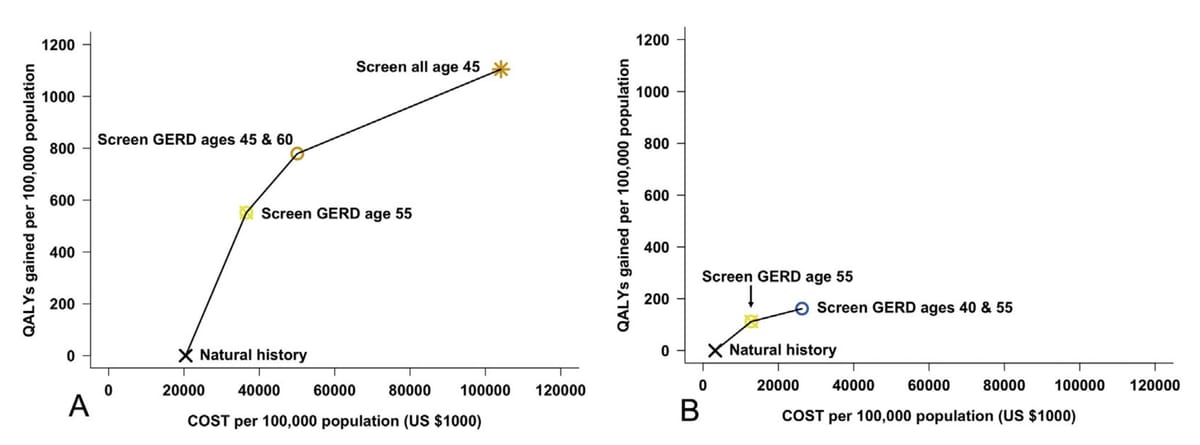
Methods: We conducted comparative cost-effectiveness analyses using 3 independent simulation models. For each combination of sex and race (White/Black, 100,000 individuals each), we considered 41 screening strategies, including one-time or repeated screening. The optimal strategy was that with the highest effectiveness and an incremental cost-effectiveness ratio <$100,000 per quality-adjusted life-year gained.
Results: Among White men, 536 EAC deaths were projected without screening, and screening individuals with GERD twice at ages 45 and 60 years was optimal. Screening the entire White male population once at age 55 years was optimal in 26% of probabilistic sensitivity analysis runs. Black men had fewer EAC deaths without screening (n = 84), and screening those with GERD once at age 55 years was optimal. Although White women had slightly more EAC deaths (n = 103) than Black men, the optimal strategy was no screening, although screening those with GERD once at age 55 years was optimal in 29% of probabilistic sensitivity analysis runs. Black women had a very low burden of EAC deaths (n = 29), and no screening was optimal, as benefits were very small and some strategies caused net harm.
Conclusions: The optimal strategy for screening differs by race and sex. White men with GERD symptoms can potentially be screened more intensely than is recommended currently. Screening women is not cost-effective and may cause net harm for Black women.
Published by Elsevier Inc.