Early age of reflux symptoms predictive of Barrett's
This study from Kaiser Permanente Northern California oberved that early onset of reflux symptoms approximately doubles risk of Barrett's esophagus, and that both severity and frequency of reflux symptoms are important in predicting risk.
J Clin Gastroenterol. 2018 Nov/Dec;52(10):873-879. doi: 10.1097/MCG.0000000000000983.
Gastroesophageal Reflux Frequency, Severity, Age of Onset, Family History and Acid Suppressive Therapy Predict Barrett Esophagus in a Large Population.
Bakr O, Zhao W, Corley D.
Abstract
GOALS: To identify risk factors associated with Barrett esophagus (BE) for potential improved surveillance and risk reduction.
BACKGROUND: Gastroesophageal reflux disease (GERD) is a known risk factor for esophageal adenocarcinoma, but the ability of GERD symptom frequency and severity to predict presence of its putative precursor lesion, BE, is less well-defined in large, community-based populations.
STUDY: We conducted a case-control study within the Kaiser Permanente Northern California population. Cases had new diagnoses of BE. To identify risk factors in the general population, we contrasted cases with population controls; to identify risk factors only among patients with GERD, we contrasted cases with GERD patients who lacked BE.
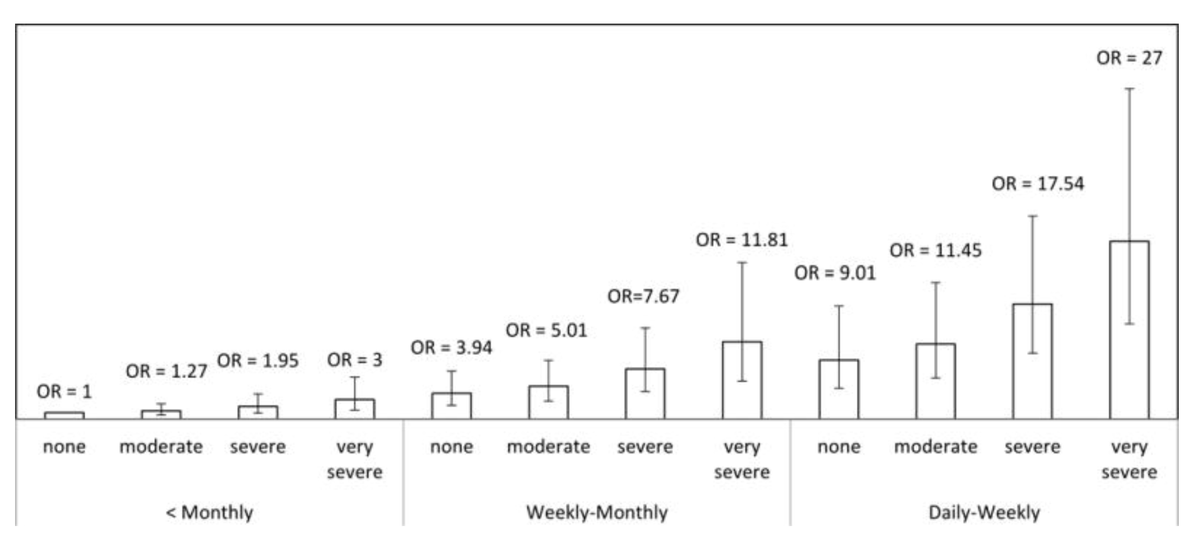
RESULTS: We interviewed 953 patients; 320 patients with BE, 316 patients with GERD who lacked BE and 317 population controls. Compared with population controls, BE risk was highest among patients with the most frequent and severe GERD symptoms [odds ratio (OR), 27.00; 95% confidence interval (CI), 14.52-50.21], nocturnal symptoms (OR, 5.40; 95% CI, 3.81-7.72), and family history of GERD (OR, 2.55; 95% CI, 1.80-3.62) or BE (OR, 10.08; 95% CI, 2.83-35.84). Although at least weekly proton pump inhibitor (PPI) use was a risk factor for BE (OR, 9.85; 95% CI, 6.54-14.84), among PPI users in the general population, GERD symptoms were not strongly associated with the risk of BE. Compared with GERD controls, cases were more likely to have onset of GERD symptoms before 30 years of age (OR, 1.93; 95% CI, 1.15-3.22) and a family history of BE (OR, 3.64; 95% CI, 1.50-8.83).
CONCLUSIONS: Severe and frequent GERD symptoms are strongly associated with increased risk of BE in the general population, especially in the absence of frequent PPI use. Among people with GERD, family history of BE and early age of symptom onset were stronger predictors of BE. These findings may improve identification of patients at highest risk for BE.