Endoscopic surveillance in rural China
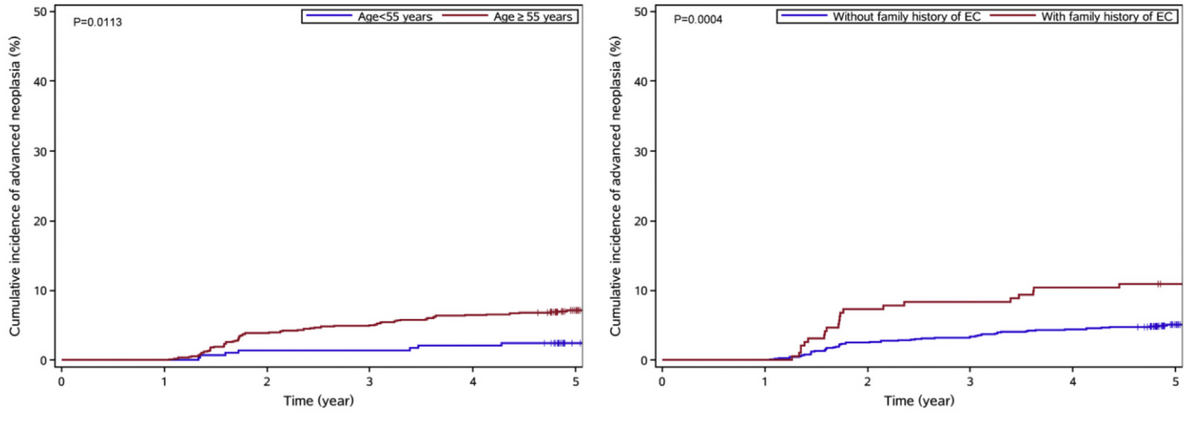
The article discusses the findings of a community-based, multicenter, prospective cohort study on endoscopic surveillance for premalignant esophageal lesions in rural China. The study aimed to assess the incidence and risk factors for advanced neoplasia in patients with mild-moderate dysplasia. The results showed that most patients with mild-moderate dysplasia stabilized or regressed to nondysplasia, with only 7.44% developing advanced neoplasia over a median follow-up time of 6.95 years. Patients with moderate dysplasia had a higher risk and shorter time interval for developing advanced neoplasia than those with mild dysplasia. Patients with mild-moderate dysplasia who had a family history of esophageal cancer and were age 55 years and older showed 97% higher advanced neoplasia yields than all patients with mild-moderate dysplasia. The authors suggested that patients with mild-moderate dysplasia should be recommended for endoscopic surveillance during the first 2 to 3 years, especially older patients or those with a family history of esophageal cancer. Further studies, including modeling studies, high-quality cohort studies, and randomized controlled trials, are needed to determine the optimal surveillance intervals for patients with premalignant esophageal lesions.
Endoscopic Surveillance for Premalignant Esophageal Lesions: A Community-Based Multicenter, Prospective Cohort Study
He Li 1, Shaokai Zhang 2, Jinyi Zhou 3, Feng Tong 4, Jiyong Gong 4, Zhenqiu Zha 5, Ni Li 1, Changfa Xia 1, Jiang Li 1, Liyang Zheng 2, Pengfei Luo 3, Renqing Han 3, Hengmin Ma 4, Yili Lv 5, Hongmei Zeng 6, Rongshou Zheng 6, Maomao Cao 1, Fan Yang 1, Xinxin Yan 1, Dianqin Sun 1, Siyi He 1, Shaoli Zhang 1, Wanqing Chen 7, Jie He 8
Abstract
Background & aims: Mild and moderate dysplasia are major premalignant lesions of esophageal squamous cell carcinoma (ESCC); however, evidence of the progression risk in patients with these conditions is extremely limited. We aimed to assess the incidence and risk factors for advanced neoplasia in patients with mild-moderate dysplasia.
Methods: This prospective cohort study included patients with mild-moderate dysplasia from 9 regions in rural China. These patients were identified from a community-based ESCC screening program conducted between 2010 and 2016 and were offered endoscopic surveillance until December 2021. We estimated the incidence of advanced esophageal neoplasia, including severe dysplasia, carcinoma in situ, or ESCC, and identified potential risk factors using the Cox regression model.
Results: The 1183 patients with mild-moderate dysplasia were followed up over a period of 6.95 years. During follow-up evaluation, 88 patients progressed to advanced neoplasia (7.44%), with an incidence rate of 10.44 per 1000 person-years. The median interval from the progression of mild-moderate dysplasia to advanced neoplasia was 2.39 years (interquartile range, 1.58-4.32 y). A total of 74.47% of patients with mild-moderate dysplasia experienced regression to nondysplasia, and 18.09% showed no lesion progression. Patients with mild-moderate dysplasia who had a family history of esophageal cancer and were age 55 years and older showed 97% higher advanced neoplasia yields than all patients with mild-moderate dysplasia.
Conclusions: In a country with a high incidence of ESCC, patients with mild-moderate dysplasia showed an overall risk of advanced neoplasia progression of 1.04% per year. Patients with mild-moderate dysplasia would be recommended for endoscopic surveillance during the first 2 to 3 years.
Keywords: Endoscopic Surveillance; Esophageal Dysplasia; Progression Rate; Risk Factors.
Copyright © 2023 AGA Institute. Published by Elsevier Inc. All rights reserved.