Gastric bypass surgery associated with reduced risk of esophageal adenocarcinoma
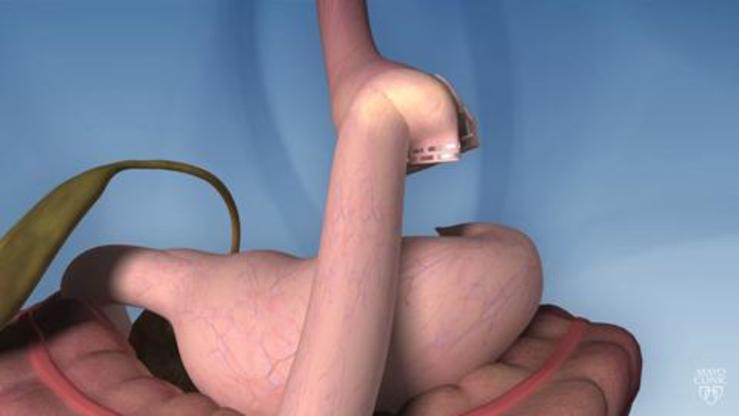
This large multinational observational study investigated whether bariatric surgery was associated with reduced risk of esophageal and cardia adenocarcinoma (ECA) in individuals diagnosed with “morbid” obesity. The study involved a cohort of almost 750,000 persons from Sweden, Finland, and Denmark, grouped based on whether they underwent bariatric surgery (n=91,731) or not. The authors observed that gastric bypass surgery was associated with a decreased risk of esophageal adenocarcinoma (but not gastric cardia cancer) over time after surgery, compared to both the background population and non-operated individuals with morbid obesity. Strengths of the study include its population-based design, relatively complete and long follow-up, and reliance on validated registries for data collection. Limitations include potential confounding by unmeasured variables (e.g., smoking, BMI, gastroesophageal reflux symptoms) and the relatively limited number of cases of esophageal adenocarcinoma (n=290 overall), which greatly reduced the precision of estimates. Overall, the authors concluded that gastric bypass surgery might mitigate the development of esophageal adenocarcinoma in individuals with morbid obesity. These results support previous research indicating a reduction in risk of obesity-related cancers after bariatric surgery.
Decreased Risk of Esophageal Adenocarcinoma after Gastric Bypass Surgery in a Cohort Study from Three Nordic Countries.
Ann Surg. 2023 Jul 14. doi: 10.1097/SLA.0000000000006003. Epub ahead of print. PMID: 37450697.
Hardvik Åkerström J, Santoni G, von Euler Chelpin M, Chidambaram S, R Markar S, Maret-Ouda J, Ness-Jensen E, Kauppila JH, Holmberg D, Lagergren J.
Abstract
Objective: To test the hypothesis that bariatric surgery decreases the risk of esophageal and cardia adenocarcinoma.
Background: Obesity is strongly associated with esophageal adenocarcinoma and moderately with cardia adenocarcinoma, but whether weight loss prevents these tumors is unknown.
Methods: This population-based cohort study included patients with an obesity diagnosis in Sweden, Finland, or Denmark. Participants were divided into a bariatric surgery group and a non-operated group. The incidence of ECA was first compared with the corresponding background population by calculating standard incidence ratios (SIR) with 95% confidence intervals (CI). Second, the bariatric surgery group and the non-operated group were compared using multivariable Cox regression, providing hazard ratios (HR) with 95% CI, adjusted for sex, age, comorbidity, calendar year, and country.
Results: Among 748,932 participants with an obesity diagnosis, 91,731 underwent bariatric surgery, predominantly gastric bypass (n=70,176; 76.5%). The SIRs of ECA decreased over time following gastric bypass, from SIR=2.2 (95% CI 0.9-4.3) after 2-5 years to SIR=0.6 (95% CI <0.1-3.6) after 10-40 years. Gastric bypass patients were also at a decreased risk of ECA compared to non-operated patients with obesity (adjusted HR=0.6, 95% CI 0.4-1.0 [0.98]), with decreasing point estimates over time. Gastric bypass was followed by a strongly decreased adjusted risk of esophageal adenocarcinoma (HR=0.3, 95% CI 0.1-0.8), but not of cardia adenocarcinoma (HR=0.9, 95% CI 0.5-1.6), when analyzed separately. There were no consistent associations between other bariatric procedures (mainly gastroplasty, gastric banding, sleeve gastrectomy, and biliopancreatic diversion) and ECA.
Conclusion: Gastric bypass surgery may counteract the development of esophageal adenocarcinoma in morbidly obese individuals.
Copyright © 2023 Wolters Kluwer Health, Inc. All rights reserved.