More evidence supporting need for individualized EA screening
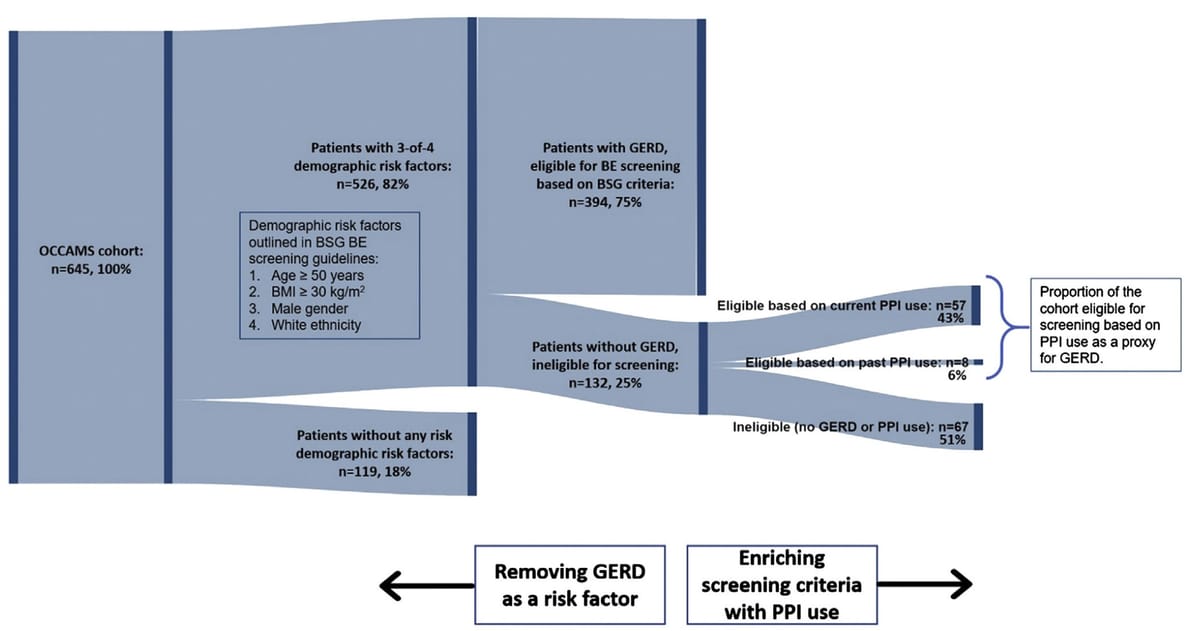
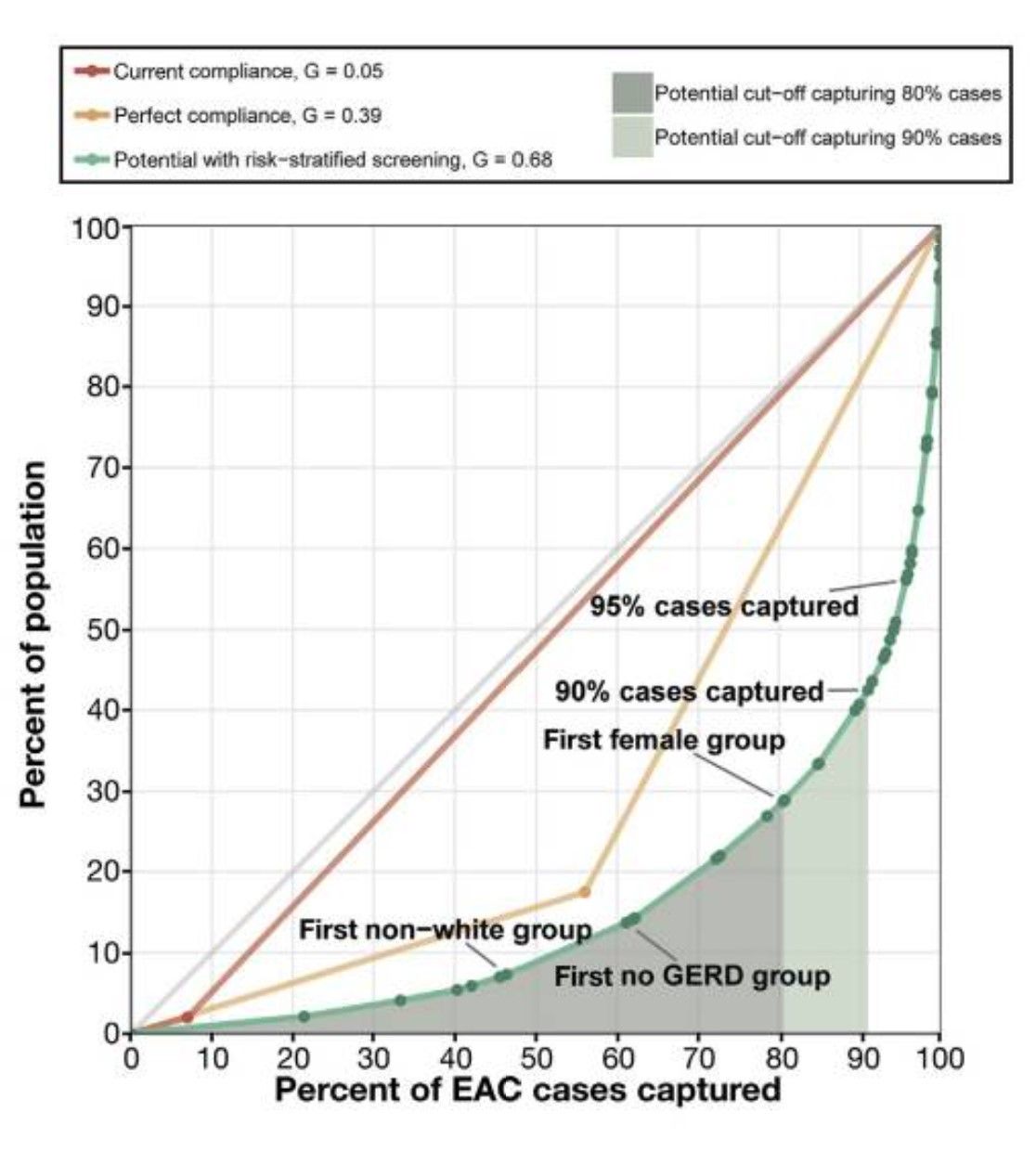
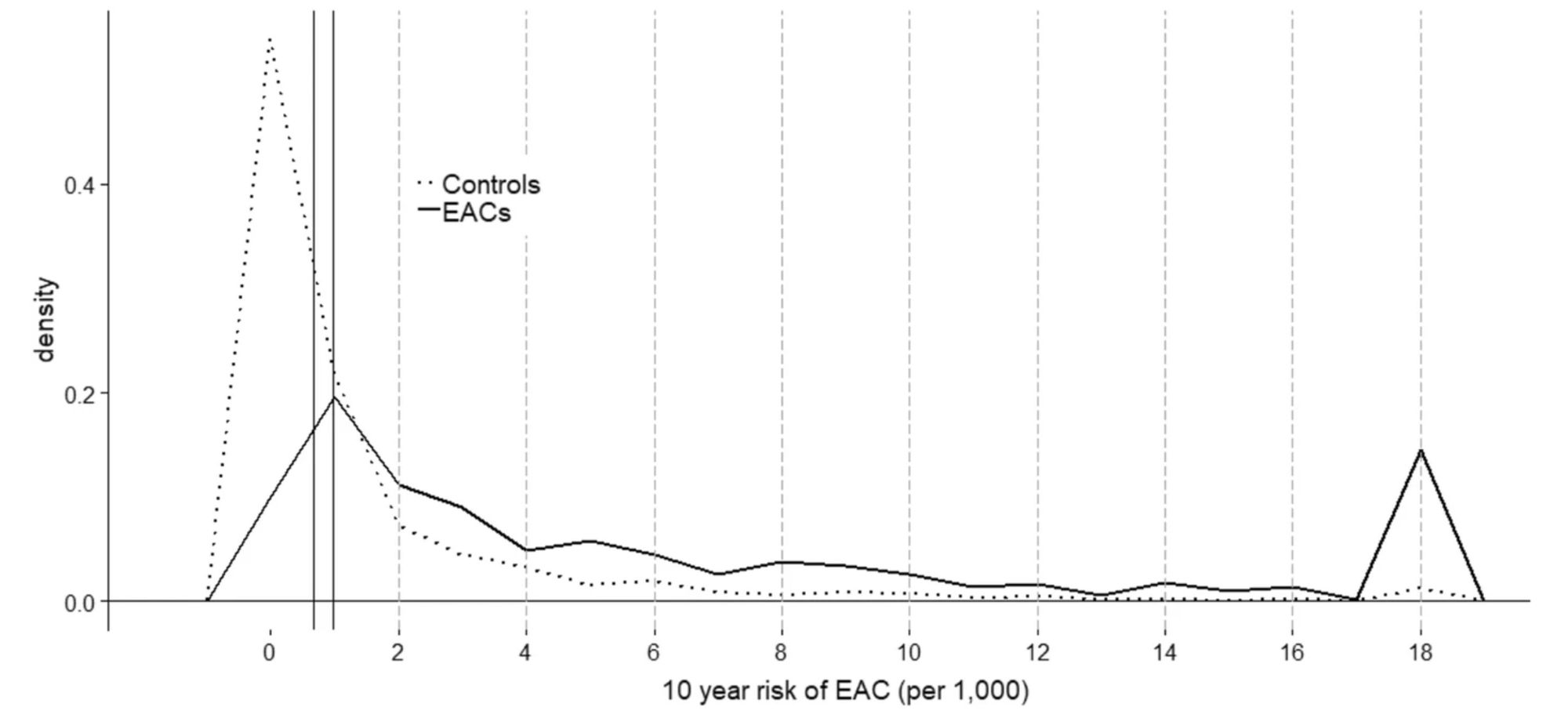
Since approximately 40% of esophageal adenocarcinoma cases arise in persons without significant gastroesophageal reflux (Nat Rev Cancer 2015), it has long been clear that screening guidelines that require GERD symptoms will miss a significant proportion of prevalent cases. Current guidelines are also inefficient with low specificity (Clin Gastroenterol Hepatol 2019.) [See figures at bottom.] This report examines ways in which screening criteria might be tweaked to increase eligibility for screening, using data from two large case series.
Clin Gastroenterol Hepatol. 2022 Aug;20(8):1709-1718.
doi: 10.1016/j.cgh.2021.10.039. Epub 2021 Oct 29.
Limitations of Heartburn and Other Societies' Criteria in Barrett's Screening for Detecting De Novo Esophageal Adenocarcinoma
Tarek Sawas 1 , Shawn A Zamani 2 , Sarah Killcoyne 3 , Andrew Dullea 2 , Kenneth K Wang 1 , Prasad G Iyer 1 , Rebecca C Fitzgerald 2 , David A Katzka 4
PMID: 34757196 DOI: 10.1016/j.cgh.2021.10.039
Abstract
Background & aims: Despite extensive Barrett's esophagus (BE) screening efforts, most patients with esophageal adenocarcinoma (EAC) present de novo. It is unclear how much of this problem is the result of insensitivity or poor applications of current screening guidelines. We aimed to evaluate the sensitivity of guidelines by determining the proportion of prevalent EAC cases that meet the American College of Gastroenterology (ACG) or the British Society of Gastroenterology (BSG) guidelines for BE screening and determine whether changes to criteria would enhance detection.
Methods: A retrospective single-center cohort from the United States (n = 663) and a prospective multicenter cohort from the United Kingdom (n = 645) were collected and analyzed independently. Screening eligibility was determined as patients with chronic reflux and at least 2 or more risk factors as defined by the guidelines. We calculated the proportion of screening-eligible patients and then compared BE/EAC risk factors between screening-eligible and screening-ineligible patients using the chi-squared or Student t test as appropriate.
Results: In the Mayo clinic cohort there were 54.9% EAC cases and in the UK cohort there were 38.9% EAC cases that were not identified by ACG or BSG screening criteria, respectively. Among patients who did not meet the screening criteria, lack of heartburn was observed in 86.5% in the Mayo clinic cohort and in 61.4% in the UK cohort. Other risk factors that were lacking included obesity (defined as a body mass index of =30 kg/m2) and family history of EAC. Eliminating chronic reflux from the ACG/BSG criteria improved eligibility for screening from 45.1% to 81.3% (P < .001) in the Mayo Clinic cohort and from 61.1% (n = 394) to 81.5% (n = 526; P < .001) in the UK cohort. However, reflux may be difficult to ascertain from the history, and by including proton pump inhibitor use status in addition to the BSG criteria, screening eligibility improved by 10.0% in the UK cohort (n = 459; P < .001).
Conclusions: ACG/BSG BE screening guidelines have limited our ability to detect prevalent EAC. An optimized approach to identifying the individuals most suitable for EAC screening needs to be implemented, particularly one that does not rely on chronic reflux symptoms.