Integration of epidemiology and machine learning in ESCC screening
The following summary made use of an accompanying comment by Drs. Dawsey and Duit:

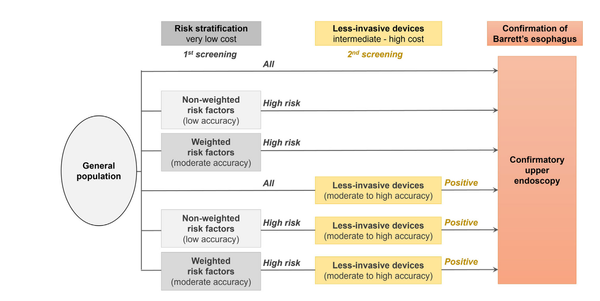
This report discusses the high prevalence of esophageal squamous cell cancer, particularly in low-income and middle-income countries, and how late onset of symptoms leads to late-stage detection and low survival rates. One potential solution is to screen high-risk individuals for early detection, but endoscopic screening is not feasible in all regions due to limited resources. This study combines questionnaire data and automated cytological evaluation of sponge-collected cells to accurately identify high-risk individuals without the need for endoscopy. The study uses machine learning to identify abnormal cells and create automated predicted risk scores that are equivalent to those of experienced cytologists. This system could potentially function with few or no cytopathologists and reduce the number of endoscopies needed to screen the population by around 90%, making it highly efficient in low-resource settings. While the study's results are promising, confirmation is needed in additional community-based studies.
Machine learning-based automated sponge cytology for screening of oesophageal squamous cell carcinoma and adenocarcinoma of the oesophagogastric junction: a nationwide, multicohort, prospective study.
Gao Y, Xin L, Lin H, Yao B, Zhang T, Zhou AJ, Huang S, Wang JH, Feng YD, Yao SH, Guo Y, Dang T, Meng XM, Yang ZZ, Jia WQ, Pang HF, Tian XJ, Deng B, Wang JP, Fan WC, Wang J, Shi LH, Yang GY, Sun C, Wang W, Zang JC, Li SY, Shi RH, Li ZS, Wang LW.
Abstract
Background: Oesophageal squamous cell carcinoma and adenocarcinoma of the oesophagogastric junction have a dismal prognosis, and early detection is key to reduce mortality. However, early detection depends on upper gastrointestinal endoscopy, which is not feasible to implement at a population level. We aimed to develop and validate a fully automated machine learning-based prediction tool integrating a minimally invasive sponge cytology test and epidemiological risk factors for screening of oesophageal squamous cell carcinoma and adenocarcinoma of the oesophagogastric junction before endoscopy.
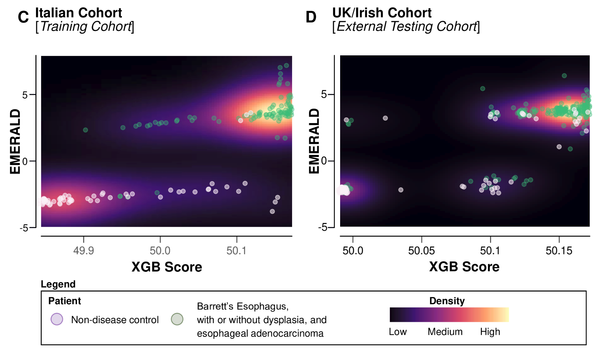
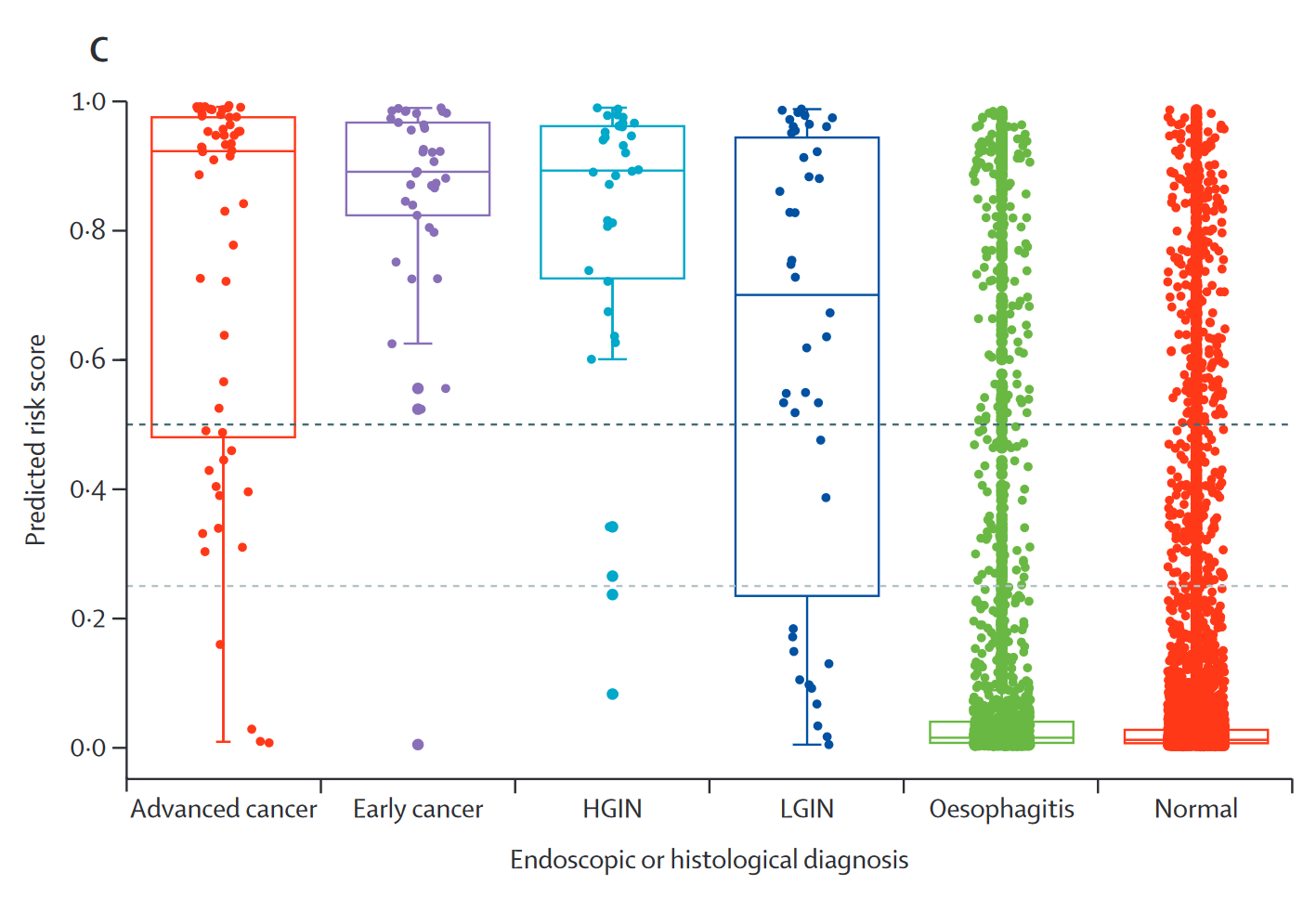
Methods: For this multicohort prospective study, we enrolled participants aged 40-75 years undergoing upper gastrointestinal endoscopy screening at 39 tertiary or secondary hospitals in China for model training and testing, and included community-based screening participants for further validation. All participants underwent questionnaire surveys, sponge cytology testing, and endoscopy in a sequential manner. We trained machine learning models to predict a composite outcome of high-grade lesions, defined as histology-confirmed high-grade intraepithelial neoplasia and carcinoma of the oesophagus and oesophagogastric junction. The predictive features included 105 cytological and 15 epidemiological features. Model performance was primarily measured with the area under the receiver operating characteristic curve (AUROC) and average precision. The performance measures for cytologists with AI assistance was also assessed.
Findings: Between Jan 1, 2021, and June 30, 2022, 17 498 eligible participants were involved in model training and validation. In the testing set, the AUROC of the final model was 0·960 (95% CI 0·937 to 0·977) and the average precision was 0·482 (0·470 to 0·494). The model achieved similar performance to consensus of cytologists with AI assistance (AUROC 0·955 [95% CI 0·933 to 0·975]; p=0·749; difference 0·005, 95% CI, -0·011 to 0·020). If the model-defined moderate-risk and high-risk groups were referred for endoscopy, the sensitivity was 94·5% (95% CI 88·8 to 97·5), specificity was 91·9% (91·2 to 92·5), and the predictive positive value was 18·4% (15·6 to 21·6), and 90·3% of endoscopies could be avoided. Further validation in community-based screening showed that the AUROC of the model was 0·964 (95% CI 0·920 to 0·990), and 92·8% of endoscopies could be avoided after risk stratification.
Interpretation: We developed a prediction tool with favourable performance for screening of oesophageal squamous cell carcinoma and adenocarcinoma of the oesophagogastric junction. This approach could prevent the need for endoscopy screening in many low-risk individuals and ensure resource optimisation by prioritising high-risk individuals.
Copyright © 2023 Elsevier Ltd. All rights reserved.