Discussion of underlying reasons for EAC/BE screening shortcomings
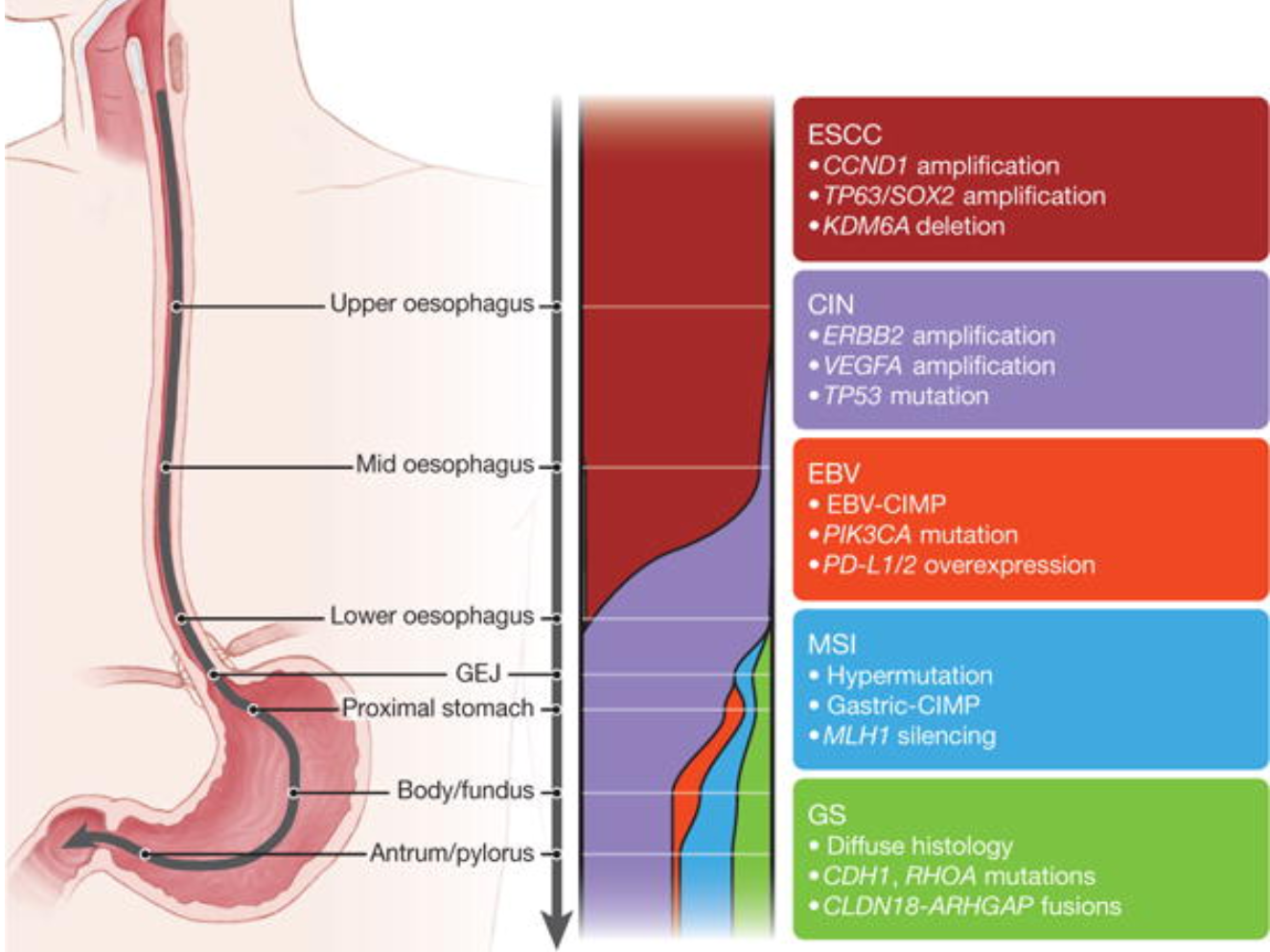
While not exactly a streetfight, Drs. Spechler and El-Serag briefly discuss in this "point/counterpoint" possible reasons that current screening approaches for esophageal adenocarcinoma and Barrett's esophagus have had only modest success in affecting incidence and mortality for this cancer. I note that neither author mentions that a roughly equal number of adenocarcinomas are diagnosed each year in the U.S. that are classified as gastric cardia even though research from the BEACON consortium suggests that many of the same risk factors for EAC affect risk of cancer arising in the gastric cardia (e.g. cigarette smoking and BMI.) This would be consistent with findings from the TCGA (The Cancer Genome Atlas) that identify many somatic genetic similarities between EAC and CIN (cancer instability) type of tumors which preferentially affect the proximal stomach (see Figure 1.)
See my summary below (there is no abstract for this article.)
Why Has Screening and Surveillance for Barrett's Esophagus Fallen Short in Stemming the Rising Incidence of Esophageal Adenocarcinoma?
Spechler SJ, Hashem B El-Serag HB
My Summary:
This article discusses the reasons behind the slow adoption of screening and surveillance for Barrett's esophagus (BE). The article notes that despite the potential benefits of detecting and treating BE early, the uptake of screening and surveillance procedures has been limited. One reason for the slow adoption of BE screening and surveillance is the lack of clear guidelines on how to perform these procedures and when to initiate them. The authors explain that while some professional organizations have issued recommendations on BE management, there is still considerable variation in clinical practice, which can lead to confusion among practitioners and patients. Another reason for the limited uptake of BE screening and surveillance is the high cost of these procedures, which can be a barrier for patients and healthcare systems. In addition, the authors argue that low reimbursement rates for these procedures can discourage physicians from offering them to their patients. The low prevalence of BE in the general population is also a factor that has contributed to the slow adoption of these practices. While BE is a risk factor for esophageal adenocarcinoma, it is relatively uncommon, and it can be difficult to identify patients who are at the highest risk of developing EAC. The article concludes that more research is needed to better understand the cost-effectiveness of BE screening and surveillance, as well as to develop more effective methods for detecting and managing this condition. In particular, the article suggests that there is a need for better risk stratification tools that can help identify patients who are at the highest risk of developing EAC, as well as for more effective surveillance strategies that can reduce the burden of unnecessary procedures for patients who are at low risk. Overall, the article highlights the need for a more coordinated and evidence-based approach to the management of BE, in order to improve outcomes for patients and reduce the burden of EAC.