Risk calculator for esophageal adenocarcinoma
This paper describes the development of the IC-RISC™ calculator and provides examples of its application in the general population and among persons with Barrett’s esophagus. (See “What’s Your Risk” menu above for the actual calculator.)
BMC Gastroenterol. 2019 Jun 27;19(1):109. doi: 10.1186/s12876-019-1022-0.
Interactive decision support for esophageal adenocarcinoma screening and surveillance.
Vaughan TL, Onstad L, Dai JY.
Abstract
BACKGROUND:
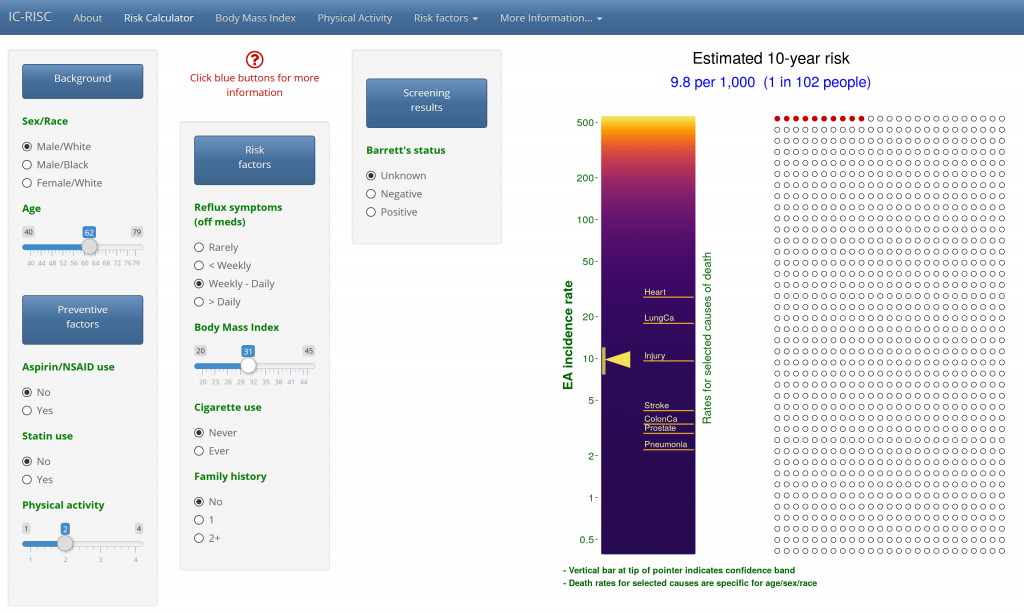
A key barrier to controlling esophageal adenocarcinoma (EAC) is identifying those most likely to benefit from screening and surveillance. We aimed to develop an online educational tool, termed IC-RISC™, for providers and patients to estimate more precisely their absolute risk of developing EAC, interpret this estimate in the context of risk of dying from other causes, and aid in decision-making.
RESULTS:
U.S. incidence and mortality data and published relative risk estimates from observational studies and clinical trials were used to calculate absolute risk of EAC over 10 years adjusting for competing risks. These input parameters varied depending on presence of the key precursor, Barrett’s esophagus. The open source application works across common devices to gather risk factor data and graphically illustrate estimated risk on a single page. Changes to input data are immediately reflected in the colored graphs. We used the calculator to compare the risk distribution between EAC cases and controls from six population-based studies to gain insight into the discrimination metrics of current practice guidelines for screening, observing that current guidelines sacrifice a significant amount of specificity to identify 78-86% of eventual cases in the US population.
CONCLUSIONS:
This educational tool provides a simple and rapid means to graphically communicate risk of EAC in the context of other health risks, facilitates “what-if” scenarios regarding potential preventative actions, and can inform discussions regarding screening, surveillance and treatment options. Its generic architecture lends itself to being easily extended to other cancers with distinct pathways and/or intermediate stages, such as hepatocellular cancer. IC-RISC™ extends current qualitative clinical practice guidelines into a quantitative assessment, which brings the possibility of preventative actions being offered to persons not currently targeted for screening and, conversely, reducing unnecessary procedures in those at low risk. Prospective validation and application to existing well-characterized cohort studies are needed.