Statins and risk of GI cancer
Evidence continues to mount from observational epidemiologic studies and animal experiments supporting the notion that statins may be effective chemopreventive agents for esophageal adenocarcinoma, and possibly useful in esophageal cancer treatment as well. In this large (over 1M persons) records-based cohort study in Korea, investigators observed a 45% reduction in esophageal cancer incidence (all histologic types) and a 59% reduction in mortality from esophageal cancer. Similar but slightly more modest reductions in incidence and mortality were also observed for gastric and colon cancers. A well-powered clinical trial of statins is urgently needed before statins can be recommended for clinical use.
J Cancer Res Clin Oncol. 2022 Oct;148(10):2855-2865. doi: 10.1007/s00432-022-04075-1. PMID: 35660949
Statins and the risk of gastric, colorectal, and esophageal cancer incidence and mortality: a cohort study based on data from the Korean national health insurance claims database.
Dong-Sook Kim, Hyun Jung Kim, Hyeong Sik Ahn
Abstract
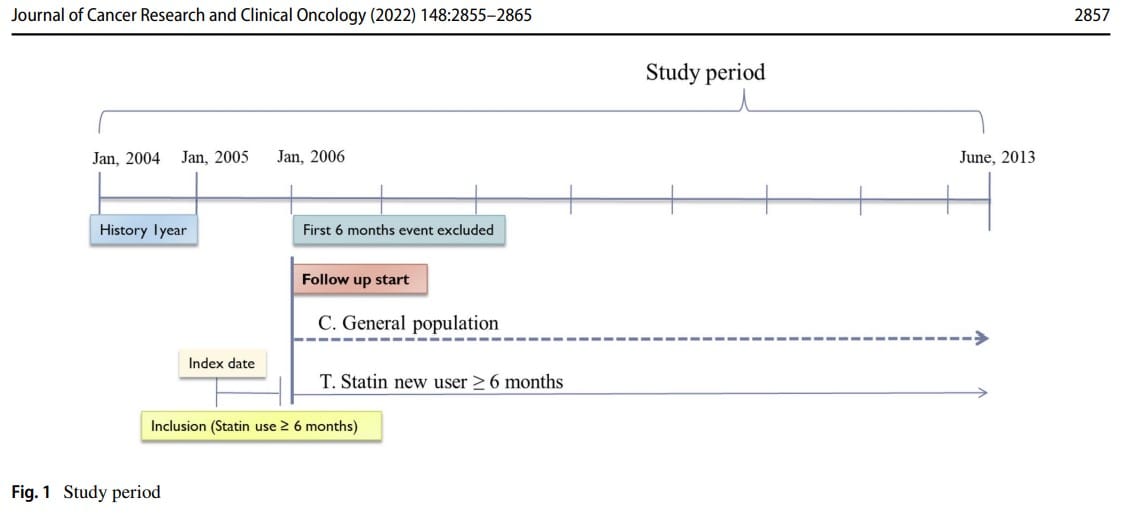
Background: This study investigated the association between the use of statins, the incidence of gastric, colorectal, and esophageal cancers, and mortality between January 2005 and June 2013 in South Korea.
Methods: We compared patients aged 45-70 years statin users for at least 6 months to non-statin users matched by age and sex, from 2004 to June 2013 using the National Health Insurance database. Main outcomes were gastric, colorectal, and esophageal cancer incidence and mortality. Cox proportional hazard regression was used to calculate the adjusted hazard ratios (aHRs) and 95% confidence intervals (95% CIs) among overall cohort and matched cohort after propensity score matching with a 1:1 ratio.
Results: Out of 1,008,101 people, 20,473 incident cancers, 3938 cancer deaths occurred and 7669 incident cancer, 1438 cancer death in matched cohort. The aHRs for the association between the risk of cancers and statin use were 0.7 (95% CI 0.65-0.74) for gastric cancer, 0.73 (95% CI 0.69-0.78) for colorectal cancer, and 0.55 (95% CI 0.43-0.71) for esophageal cancer. There were associations between statin use and decreased gastric cancer mortality (HR 0.46, 95% CI 0.52-0.57), colorectal cancer mortality (HR 0.43, 95% CI 0.36-0.51), and esophageal cancer mortality (HR 0.41, 95% CI 0.27-0.50) in the overall cohort and this pattern was similar in the matched cohort.
Discussion: Statin use for at least 6 months was significantly associated with a lower risk of stomach, colorectal, and esophageal cancer incidence as well as cancer mortality after a diagnosis.