When to stop Barrett's surveillance?
Gastroenterology societies recommend surveillance for non-dysplastic Barrett's but do not give guidance on when to stop. This modeling study suggests that the optimal age for last surveillance of NDBE patients depends on the sex and the comorbidity level of patients.
Gastroenterology. 2021 May 8;S0016-5085(21)00751-4.
doi: 10.1053/j.gastro.2021.05.003. Online ahead of print.
The optimal age to stop endoscopic surveillance of Barrett's esophagus patients based on sex and comorbidity: a comparative cost-effectiveness analysis
Amir-Houshang Omidvari 1 , William D Hazelton 2 , Brianna N Lauren 3 , Steffie K Naber 4 , Minyi Lee 5 , Ayman Ali 6 , Claudia Seguin 5 , Chun Yin Kong 5 , Ellen Richmond 7 , Joel H Rubenstein 8 , Georg E Luebeck 2 , John M Inadomi 9 , Chin Hur 3 , Iris Lansdorp-Vogelaar 4
PMID: 33974935
Abstract
Background & aims: Current guidelines recommend surveillance for non-dysplastic Barrett's esophagus (NDBE) patients but do not include a recommended age for discontinuing surveillance. This study aimed to determine the optimal age for last surveillance of NDBE patients stratified by sex and level of comorbidity.
Methods: We used three independently developed models to simulate patients diagnosed with NDBE, varying in age, sex, and comorbidity level (no, mild, moderate, severe). All patients had received regular surveillance until their current age. We calculated incremental costs and quality-adjusted life-years (QALYs) gained from one additional endoscopic surveillance at the current age versus not performing surveillance at that age. We determined the optimal age to end surveillance as the age at which incremental cost-effectiveness ratio (ICER) of one more surveillance was just below the willingness-to-pay threshold of $100,000/QALY.
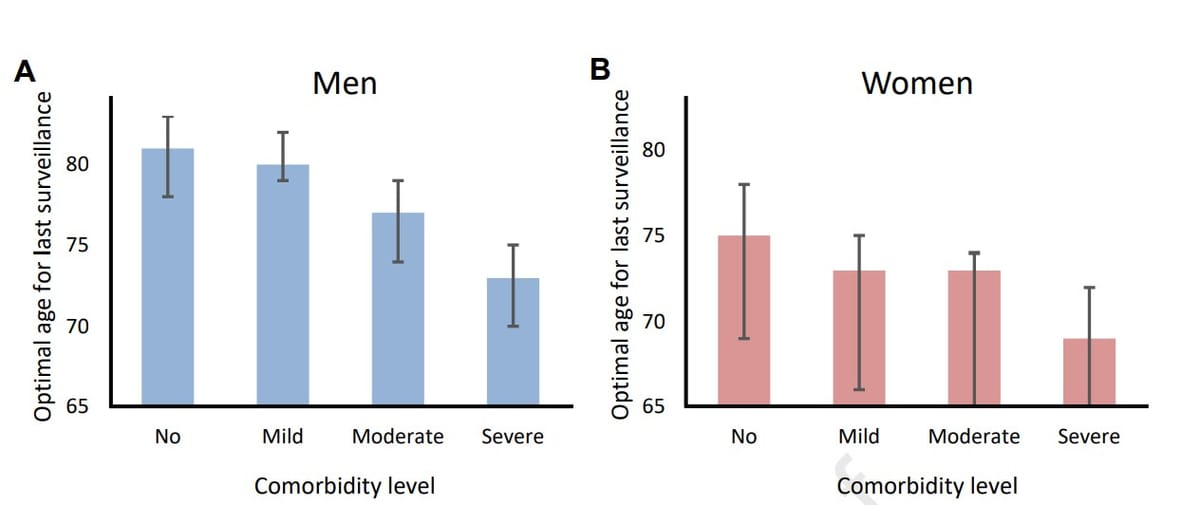
Results: The benefit of having one more surveillance endoscopy strongly depended on age, sex and comorbidity. For men with NDBE and severe comorbidity, one additional surveillance at age 80 years provided 4 more QALYs per 1,000 BE patients at an additional cost of $1,2 million, while for women with severe comorbidity the benefit at that age was 7 QALYs at a cost of $1.3 million. For men with no, mild, moderate and severe comorbidity, the optimal ages of last surveillance were 81, 80, 77 and 73 years, respectively. For women, these ages were lower: 75, 73, 73 and 69 years, respectively.
Conclusions: Our comparative modeling analysis illustrates the importance of considering comorbidity status and sex when deciding upon the age to discontinue surveillance in patients with NDBE.
Copyright © 2021 AGA Institute. Published by Elsevier Inc. All rights reserved.