Bariatric surgery vs medications in Barrett's
Does bariatric surgery influence subsequent risk of esophageal adenocarcinoma? Depending on whom and when you ask, what population or subpopulation you study, and which surgical procedures are considered, studies variously suggest no effect, increased risk and reduced risk. Moreover, some of the apparently discrepant results originate from the same author groups and study populations. In an Annals of Surgery article recently reviewed here (1), Åkerström, et al., reported that “gastric bypass surgery is followed by a decreased risk of ECA over time after surgery both compared to the corresponding background population and nonoperated patients with morbid obesity.” Two months later, they reported that “in this cohort of patients with Barrett’s esophagus, the risk of esophageal adenocarcinoma (EA) did not decrease after antireflux surgery compared to antireflux medication. Instead, the risk was increased throughout the follow-up...”
Confused? It's unfortunate that the authors didn’t directly address these apparently discrepant results, but both conclusions may have validity. The first study included persons not known to have Barrett’s esophagus (BE) but with morbid obesity, most of whom would be likely to have severe GERD (reflux) symptoms, putting them at substantial risk of EA. In such a group, bariatric surgery may indeed reduce risk via reduced reflux and weight resulting in lower systemic and localized inflammation. The second study, in contrast, included only persons with BE, who already have metaplastic changes in their esophagus that put them at a much higher baseline risk of progression to EA (see risk calculator.) In those who already have BE, GERD and obesity are less predictive of EA; thus an intervention that targets weight and reflux is less likely to reduce risk, especially when compared to persons already being treated with anti-reflux medication. Additional limitations of the second study include i) a disproportionate fraction of surgery patients from Finland (53.1% vs 16.5% of the non-surgery patients), magnifying any biases that might exist related to different selection of patients for surgery and follow up; ii) a small number (n=14) of EA patients in the surgery group, of which only 10 had been followed for five or more years; and iii) inability to control for the key risk factors for progression in BE patients: BMI or other measures of obesity, GERD symptoms, anti-reflux medication use, BE segment length and dysplasia status.
In conclusion, the potential for decreased risk of EA should probably not be a prime motivating factor for bariatric surgery given the low absolute risk in persons without BE. Among persons with BE, I feel that the results are over-interpreted, and much more research is needed to determine its influence. These questions may soon become moot with the rapidly-increasing use of weight reduction medications, which will need to be studied in the future.
Comments? tvaughan@uw.edu
1. Ann Surg. 2023 Dec 1;278(6):904-909. doi: 10.1097/SLA.0000000000006003. Epub 2023 Jul 14.
2. Gastroenterology. 2023 Sep 9:S0016-5085(23)04980-6. doi: 10.1053/j.gastro.2023.08.050.
Antireflux Surgery Versus Antireflux Medication and Risk of Esophageal Adenocarcinoma in Patients With Barrett's Esophagus.
Åkerström JH, Santoni G, von Euler Chelpin M, Ness-Jensen E, Kauppila JH, Holmberg D, Lagergren J.
Abstract
Background & aims: Antireflux treatment is recommended to reduce esophageal adenocarcinoma in patients with Barrett's esophagus. Antireflux surgery (fundoplication) counteracts gastroesophageal reflux of all types of carcinogenic gastric content and reduces esophageal acid exposure to a greater extent than antireflux medication (eg, proton pump inhibitors). We examined the hypothesis that antireflux surgery prevents esophageal adenocarcinoma to a larger degree than antireflux medication in patients with Barrett's esophagus.
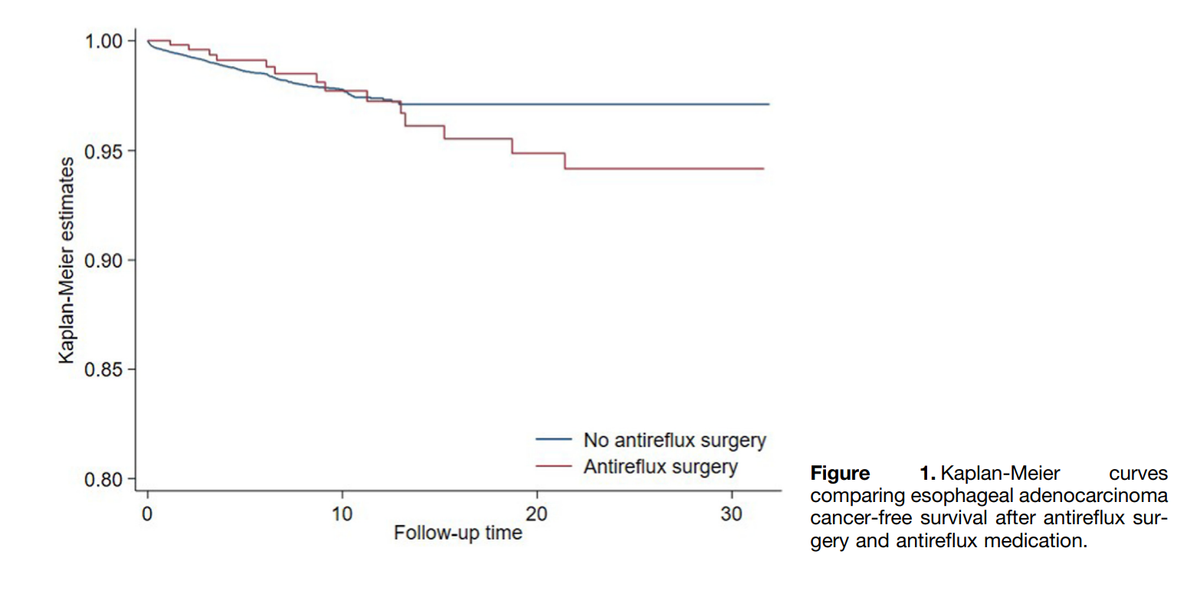
Methods: This multinational and population-based cohort study included all patients with a diagnosis of Barrett's esophagus in any of the national patient registries in Denmark (2012-2020), Finland (1987-1996 and 2010-2020), Norway (2008-2020), or Sweden (2006-2020). Patients who underwent antireflux surgery were compared with nonoperated patients using antireflux medication. The risk of esophageal adenocarcinoma was calculated using multivariable Cox regression, providing hazard ratios (HRs) and 95% CIs adjusted for age, sex, country, calendar year, and comorbidity.
Results: The cohort consisted of 33,939 patients with Barrett's esophagus. Of these, 542 (1.6%) had undergone antireflux surgery. During up to 32 years of follow-up, the overall HR was not decreased in patients having undergone antireflux surgery compared with nonoperated patients using antireflux medication, but rather increased (adjusted HR, 1.9; 95% CI, 1.1-3.5). In addition, HRs did not decrease with longer follow-up, but instead increased for each follow-up category, from 1.8 (95% CI, 0.6-5.0) within 1-4 years of follow-up to 4.4 (95% CI, 1.4-13.5) after 10-32 years of follow-up.
Conclusions: Patients with Barrett's esophagus who undergo antireflux surgery do not seem to have a lower risk of esophageal adenocarcinoma than those using antireflux medication.