Why Don't We Get Counseling?

This article addresses an interesting question: why are Barrett's esophagus patients not offered specialist counseling in much the same way as persons carrying genetic mutations (e.g., BRCA1/2) that confer increased cancer risk? Dr. Davies examines the contrasting approaches in UK NICE guidelines regarding psychosocial support for patients diagnosed with these two conditions, observing that while genetic risk patients receive counseling and psychosocial care due to factors like higher cancer risk, familial implications, and historical emphasis on genetic exceptionalism, patients with morphological risks often lack similar support despite experiencing comparable emotional distress. The paper argues for expanding care models for morphological risk conditions by integrating lessons from genetic counseling to better address patients' psychosocial needs and calls for further research to optimize clinical practices within resource constraints.
'Why Don't We Get Counselling?': Comparing NICE Guidelines for Morphological and Genetic Cancer Risk Diagnoses.
Cancer Med. 2025 Jan;14(2):e70607. doi: 10.1002/cam4.70607. PMID: 39812114; PMCID: PMC11733675.
Davies E.
ABSTRACT
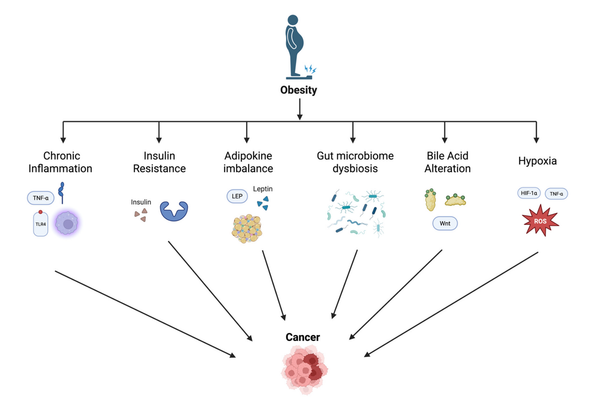
Background: In the UK's National Health Service (NHS), there is specific psychosocial care offered to people with genetic cancer risk conditions but not morphological cancer risk conditions. As researchers develop new ways to diagnose morphological risk conditions, including pre-cancers and in situ cancers, it is important to consider the psychosocial care that those diagnosed might require.
Objectives: This study compares the National Institute for Health and Care Excellence's guidelines for BRCA1/2, which are genetic risk conditions, and Barrett's oesophagus (BO), a morphological risk condition. It then theorizes reasons for the similarities and differences made visible by this comparative work.
Methods: The author completed an in-depth analysis of two sets of NICE guidelines, before carrying out a review of historical and social scientific literature on cancer risk to offer potential explanations for the disparities identified.
Results: The ‘right not to know’ is protected in the case of BRCA1/2 diagnoses, but not BO. Additionally, specialist counseling is required for people receiving diagnoses of genetic risk but not offered for those diagnosed with morphological risk conditions. The paper offers four possible reasons for these disparities, concluding that they appear to be in large part due to historic genetic exceptionalism, rather than differences in patients' needs.
Conclusion: There may be a need to consider offering further psychosocial care to people with morphological risk conditions like BO. Lessons might be learnt from the field of genetic counselling.