research
Best practice guidelines for reducing use of PPIs
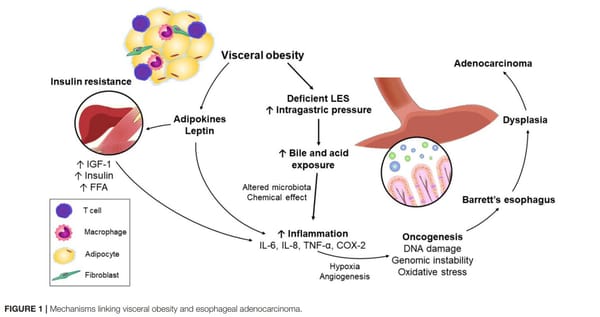
Proton pump inhibitors (PPIs) are commonly used to treat reflux, a key risk factor for esophageal adenocarcinoma. However, they have the potential for side effects. This expert review provides "best practice advice" for de-prescribing PPIs. Gastroenterology. 2022 Feb 16;S0016-5085(21)04083-X. doi:10.1053/j.gastro.2021.